- Taiwan says four employees of Apple supplier Foxconn arrested in China
- What internet data brokers have on you — and how you can start to get it back
- Cramer wants to buy more of this chipmaker, considers adding another cybersecurity stock
- Pharmacy deserts are appearing across U.S. as Rite Aid, Walgreens, CVS drug store closures spread
- Ozempic is driving up the cost of your health care, whether you can get your hands on it or not
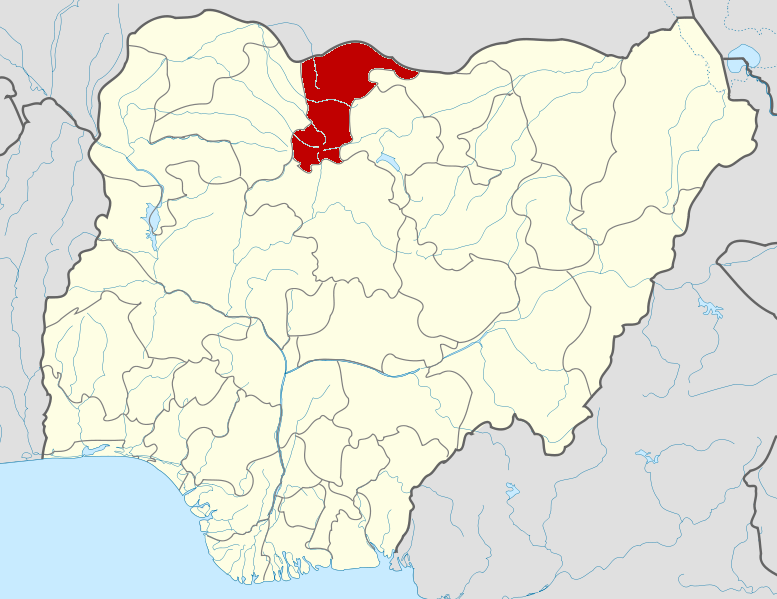
What do you believe is the single most important factor driving up the cost of living in Nigeria?

Ozempic is driving up the cost of your health care, whether you can get your hands on it or not
About 165 million Americans rely on employer-sponsored health insurance, and yet workers may still not get the coverage they want — particularly when it comes to drugs such as Novo Nordisk's weight-loss drug Wegovy and diabetes drug Ozempic.
About 1 in 3 employees are looking for more resources to combat obesity, according to a recent report by consulting firm Gallagher. Glucagon-like peptide-1 treatments such as Wegovy and Ozempic, which mimic hormones produced in the gut to suppress a person's appetite, are considered game changers on this front.
These blockbuster weight-loss drugs have skyrocketed in popularity in the U.S. but are still not universally covered — even though "Americans have higher rates of obesity and diabetes and more behavioral health conditions today than ever before," according to Trilliant Health's "2024 Trends Shaping the Health Economy" report.
Cost is a key issue.
Although research shows that obesity drugs may have significant health benefits beyond shedding unwanted pounds, organizations representing U.S. insurers have said concerns remain about the high price involved in covering those medications, which are nearly $1,350 per month for a single patient.
More from Personal Finance:
- October 11, 2024
Katsina enrols 386,289 people into contributory healthcare scheme



- October 11, 2024
Schneider Electric launches new solutions

- October 11, 2024
Bat data study reveals conservation priorities in San Diego County




- October 11, 2024
Parents advised not to hide children with down syndrome
Subscribe to our mailing list to get the new updates!

Subscribe our newsletter to stay updated
Thank you for subscribing!





